Scientists are turning to CRISPR, viruses, designer molecules, and protein swords as alternatives to traditional antibiotics, which can lead bacteria toward drug resistance.
It is possible that the bacteria entered her skin along with shrapnel after the bomb detonated at Brussels Airport in 2016. The microbes could have been carried on surgical instruments to treat the wounds. The “superbug” resisted being eradicated despite years and years of antibiotic treatments.
She had survived a terrorist assault but was still held hostage by drug-resistant Klebsiella pneumoniae, a bacterial strain often contracted by hospital surgery patients. Doctors could only rid the woman of her superbug by combining antibacterial drugs with an experimental new treatment.
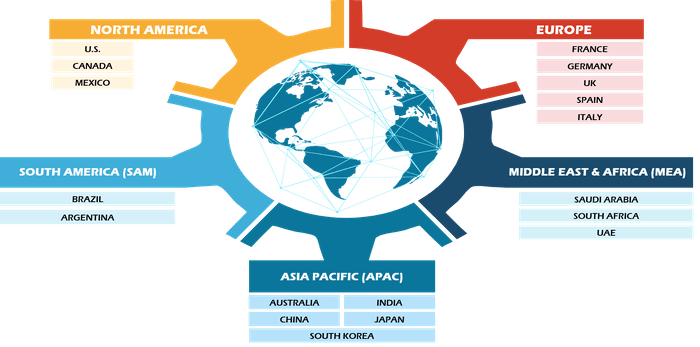
Drug-resistant bacteria are a growing threat to the global health. Antibiotic-resistant bacteria killed approximately 1.27 million people in 2019 and contributed to another 3.68 million deaths. Drug-resistant bacteria, fungi, and viruses cause about 2.8 million infections in the U.S. and 35,000 deaths yearly.
You can boost your food powder production in more than one way.
The problem is only getting worse. Seven out of 18 bacteria that the Centers for Disease Control and Prevention track are increasingly resistant to antibiotics, vital for maintaining public safety. Drug companies still need to be faster in developing new antibiotics that can beat the microbes. According to the World Health Organization, only 30 of the more than 300 antibiotics in development are targeted at “priority” microbes. Most of these drugs, however, still face resistance.
Scientists are now looking for alternatives to traditional antibiotics that will not fuel the growth of superbugs. The new arsenal includes viruses that kill bacteria, CRISPR, and molecules that destroy microbes. These experimental treatments, which some have tested on patients, are hoped to kill superbugs while preventing resistance.
Live Science reported that Chase Beisel is the RNA Synthetic Biology research group leader at Germany’s Helmholtz Institute of RNA-based Infection Research.
Experts say that the overuse and misuse of antibiotics are accelerating the rate of their obsolescence.
Antibiotic resistance: how it develops and spreads
Antibiotics can either kill bacteria directly or slow down their growth. The immune system then finishes the job. These drugs can work in various ways, such as by stopping bacteria from building strong walls or replicating their DNA. Antibiotics that slow growth usually affect ribosomes – the factories where bacteria make proteins.
The mechanisms of many antibiotics are the same, and they are universal enough to work against both gram-positive and gram-negative bacteria, which differ in their cell wall thickness and makeup. Broad-spectrum antimicrobials, in particular, force harmful and beneficial bacteria to develop defensive strategies that eject, disable, or alter the targets of the drugs.
Bacteria may acquire such defenses by acquiring random mutations in DNA or swapping the “resistance gene” with another bacterium via a horizontal gene transfer process. These gene transfers allow bacteria to spread conversions in the body or the environment quickly.
Antibiotics misused in the health care system, as well as in agriculture, have given bacteria a lot of opportunities to develop resistance. This increases the risk that infections, once treatable, will become deadly.
Use viruses to combat bacteria.
The idea of an alternative to antibiotics began more than a hundred years ago, long before the discovery of penicillin in 1928. Phage therapy uses bacteria-infecting viruses called bacteriophages or “phages” that kill germs by invading and slicing open their cells from the inside.
Phages can also force bacteria to give up essential tools in their toolkits of drug resistance. This can be achieved by a phage named U136B, for example. The phage infects E. coli by using an efflux pump, a protein that E. coli uses to pump out antibiotics from the cell. The E. coli will reduce its ability to pump antibiotics out if it tries to alter this pump to escape the virus.
Paul Turner, Director of the Center for Phage Biology and Therapy at Yale University, says that, unlike antibiotics, bacteria will not develop widespread resistance to phage treatment.
Turner and other experts concluded that “if phage treatment were used globally, it would not cause the same widespread resistance problem as antibiotic use,” he said to Live Science.
The misuse and overuse of antibiotics have dramatically increased antibiotic resistance, particularly broad-spectrum antibacterials, which work on many bacteria. Phages can target much more specific targets than narrow-spectrum antimicrobials, such as a protein only found in a small number of strains or bacteria within a single species.
Related: New drugs can stop superbugs from evolving by freezing their evolution
Turner explained that while the target bacterium may still be able to evolve resistance against a single phage, scientists could make the bacterium’s evolution come at a price by selecting the right combination. This could be in the form of a reduction in virulence or an increased vulnerability to antibiotics.
Phage therapy has been primarily tested in a regulatory framework called “compassionate usage” on patients such as the Brussels Airport bombing victims, who had no other options for treatment. In these situations, phage therapy has been successful. A recent observational study of over 100 patients treated with phages and antibiotics also showed success.
Phage therapy isn’t more effective than standard antibiotics or even a placebo in clinical trials. Two recent studies have shown promising results in treating specific foot and lung infections. However, the full results are still pending.
Turner stated that the success of future trials is crucial to bringing phages to clinics. Turner said the problems would have to prove the therapy is effective for different infections, establish dosage, and confirm that phage treatments don’t harm helpful bacteria.
Antibacterial defenses can be turned against bacteria.
The CRISPR technology, although widely known as a powerful tool for gene editing, was adapted by CRISPR Cas. This immune system is found in many bacteria.
This immune system comprises molecular scissors (Cas proteins) and a bank of DNA fragments collected by phages that infected the bacterium. CRISPR Cas’s memory bank allows it to guide its lethal scissors at a precise spot in the DNA of an invading virus and snip that point like a ribbon.
The CRISPR machine enters a group of cells, but only those with the sequence or sequences that you selected will be attacked. In some cases, however, instead of attacking phages, CRISPR Cas may accidentally attack the DNA of a bacterial cell, triggering an autoimmune reaction. Beisel’s and his co-workers’ curiosity about this phenomenon led them to investigate the possibility of using CRISPR to shred DNA from bacterial cells.
Beisel, a Live Science reporter, said that the tool’s natural appeal is its sequence-specificity, which means it only targets DNA sequences you specify, not other sequences in bacteria. Once administered to a person, the CRISPR machine will enter a group of cells. But only those with the chosen sequence or sequences will be killed.
How can you deliver CRISPR-Cas to the correct bacteria? Beisel explained that different research groups are testing various delivery methods. However, currently, the best strategy is to load CRISPR machinery in a phage that infects the target bacteria.
Beisel, also a scientific advisor at Locus Biosciences (a biotech firm), is currently testing CRISPR-enhanced Phage Therapy in a mid-stage trial involving about 800 people. This approach combines the bacteria-killing abilities of phages and the ability of CRISPR Cas to destroy essential genes in bacteria. Clinical trials are required to determine the safety profile of CRISPR-less therapies and their appropriate dosage.